Chiropractic care of a 10-year-old female with primary nocturnal enuresis: a case report
By Anissa St-Jean, DC1
1. Private Practice of Chiropractic, Hawkesbury, Ontario, Canada
Email: astjeanchiro@gmail.com, 438-888-1858
Funding Sources and Potential Conflicts of Interest: No funding sources or conflicts of interest were reported for this study.
ABSTRACT
Introduction: Nocturnal enuresis is a common pediatric condition with low scientific value in literature. Nocturnal enuresis is a frequent complaint of patients who present to chiropractic clinics. Early management can often avoid the development of socially disruptive and stressful conditions in the future. The purpose of this study is the resolution of nocturnal enuresis in a 10-year-old female patient after receiving chiropractic care. Design architecture: Case report. Methods: Databases searched were PubMed, Mantis, Cochrane, Index to Chiropractic Literature, CINAHL and google scholar. Keywords were nocturnal enuresis, bedwetting, chiropractic, child and conservative management. Presenting concerns: A 10-year-old female child presented to the chiropractor’s office alleging constant night-time bedwetting. This condition affected the self-esteem of the patient. Behavioral and medical approaches were unsuccessful. Interventions: The outcome measures assessed were the amount of urination (little, moderate or full diapers) against dry nights and the patient’s overall sense of well-being rated on a global well-being scale. The patient completed the initial questionnaire and responded to the diagnostic criteria for nocturnal enuresis. A chiropractor performed an exhaustive history and spinal examination. The patient was treated on 14 occasions over 10 weeks. Throughout the 10 weeks, the patient kept a diary to record the number of wet and/or dry nights per week and a global well-being scale was completed at every second week until the end of the treatment plan. Outcomes: Results show a decline in nocturnal enuresis and at the end, complete resolution. Also, there was a positive change in the global well-being scale score of 10/10 by the end of the treatment plan. Conclusion: It appears that chiropractic treatment may have a role in the improvement of nocturnal enuresis.
Keywords: nocturnal enuresis, bedwetting, chiropractic, child and conservative management.
Introduction
Musculoskeletal conditions represent the most common chiropractic care visits in private clinics according to Humphreys et al (2007)1 while the National Center of Health Statistics found that in the United States (2007), a large variety of other pediatric health conditions are also presenting in chiropractic clinics.2 Enuresis is one of the issues that leads parents to seek complementary and alternative medicine (CAM) practitioners.2 Nocturnal enuresis (NE) can be defined by the involuntary loss of urine during sleep, without organic disease at a developmental age of 5 years or older.3 NE occurs in 15% to 20% of children of five years of age, 5% of children of 10 years of age and 1% to 2% of those 15 years and older.3 Numerous causes could be associated with NE but it is yet not clear.3 Some factors that could contribute to it include physiological, psychological, genetic, or neurological developmental delays and the consumption of a diet or drinks with diuretic effects. Without any treatment, about 15% of bedwetting children are cured each year.4 The most commonly used treatments are pharmacological interventions (e.g., desmopressin, tricyclic drugs and many other drugs)5-7 and behavioral interventions (reward systems and alarms).8-10 According to Maternik et al, alarm therapy is curative in 60% of children through conditioning effects on arousal and/or increasing bladder volume and approximately 70% of patients respond to desmopressin, but a high recurrence rate is observed following cessation of this therapy.11 Both methods are equivalent first-line treatment options which can be proposed by the general practitioner. Alternative treatments such as acupuncture, homeopathy, hypnosis and chiropractic also exist.3 Only two randomized controlled trials (RCTs) on chiropractic interventions have been published.12,13 These trials suggest that there is a weak evidence for its effectiveness due to a randomization bias, lack of a strict treatment protocol and small trial according to the most recent publication by Hang and all three who have performed a Cochrane Database System review of all complementary and miscellaneous interventions for nocturnal enuresis in children.
Bedwetting can lead to a social and emotional stigma and reduce the quality of life for the patient.3 It may consequently affect the self-esteem of those with NE and generate stress factors for them and their families.3 However, early management can often prevent the development of socially disruptive stressful conditions in the future. Chiropractors receive patients with this condition in their clinic, and each child requires an individualized approach using best evidence. Therefore, the aim of this study is to document the resolution of nocturnal enuresis in a 10-year-old female patient after receiving chiropractic care. The outcome measures assessed were the change in the factors that diagnostically define NE and the patient’s overall sense of well-being.
Reviews of the literature
To help present the chiropractic management and care of children with NE, a review of the literature were performed on the field. Using PubMed, Mantis, Cochrane, Index to Chiropractic Literature, CINAHL and google scholar. No date limit for studies were applied. Using the following keyword search: nocturnal enuresis OR bedwetting AND chiropractic AND child AND conservative management. Selection criteria were publication published in a peer-reviewed with English or French language journal, the population was 18 years old or younger and the subject related to chiropractic care of patient with NE in relation to bedwetting. Also, studies with other main complaints were excluded for example incontinence or constipation. Our literature search resulted with six case reports,14-19 one literature review,20 one cohort,12, one case series,21 one clinical trial13 and five systematic reviews3,10,22-24 on the two randomized controlled trials (RCTs).
Only two trials have been published on enuresis involving 171 and 46 children respectively.12,13 Spinal manipulation was performed by chiropractors only. The first trial by Leboeuf and colleagues reported inconclusive evidence for the effectiveness of chiropractic intervention for NE over other common types of therapy. The second trial revealed that the study results strongly suggest the effectiveness of chiropractic treatment for primary nocturnal enuresis by reducing bedwetting by 50 in 25% of patients in the chiropractic adjustment group compared to the nonresponsive group who concluded no improvement. Our literature searches were limited on this topic to document the chiropractic care of children with NE.
Case Presentation
The design of the study was in the form of a case report. The subject was a 10-year-old, Caucasian female brought in by her mother for an initial chiropractic evaluation seeking a second opinion about her unsuccessfully treated night-time bedwetting. The patient reported never experiencing a dry night. The quantity of urine was more abundant when she would sleep outside the home or when she would experience stress factors at school and when she was sick or tired. The child had no history of traumas, accidents or other injuries. There was no family history of NE declared or other comorbidities or complaints regarding the spine. During the chiropractic consultation, the mother reported that she was concerned for her daughter’s self-esteem as well. Her daughter has slept with pull-up diapers on since she was five years old. As their first choice of treatment, the mother tried behavioral therapy for a couple of weeks, which included waking her daughter up twice per night to urinate and avoid drinking after dinner but this approach was ineffective. Her primary medical doctor treated her with 60 ug of desmopressin once per day for 12 weeks without, unfortunately, any change in her bedwetting. Prior to the prescription of medication, the doctor had ruled out any abnormalities and organic cause by performing an ultrasound and urine tests who include, urinalysis and urine culture.
Physical Examination
The chiropractic examination revealed an unremarkable neurological and orthopedic examination. Motion palpation revealed a fixation of the posterior sacral base on the right side. There was also a palpable hypertonicity of the psoas muscle bilaterally. Visual postural examination revealed hyperlordosis of the lumbar spine.
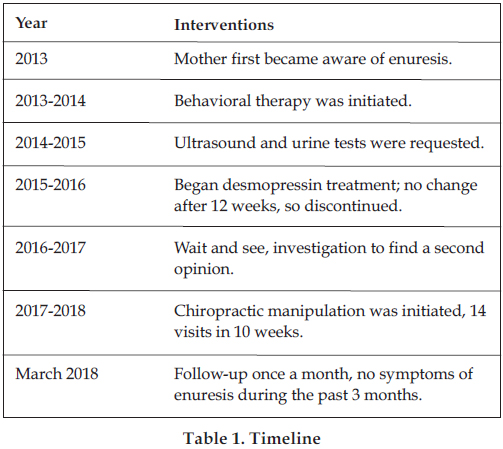
The timeline (Table 1) shows the different interventions that were initiated chronologically.
Diagnostic Assessment
It is not necessarily difficult to diagnose enuresis for health professionals, however, evaluating structure and function is important for the chiropractor to formulate an effective treatment plan. Many classifications and definitions of NE exist in the literature seen in previous years. The classification systems differentiate enuresis happening during the day versus occurring only at night, whether there were any organic diseases involved and/or whether there was a period of time in which the patient experienced dry nights before the onset of bedwetting.25 In this case, the patient’s history should distinguish daytime voiding symptoms, as well as the frequency and timing of enuresis to differentiate between monosymptomatic (bedwetting and nocturia being the only symptoms) and non-monosymptomatic enuresis (incontinence, frequency, urgency, low-voided volume).25 A distinction must also be made between primary enuresis which is defined as a child that was never “dry” for longer than six consecutive months, whereas the term secondary enuresis is used for enuresis symptoms with new onset after a dry period of six months.26
Urinary incontinence can be related to numerous renal or neurological pathologies and metabolic diseases.25 Due to the complexity of the differential diagnosis, it require a collaborative evaluation for ruling out pathology as well as any structural cause of enuresis. Urine tests can be useful, most common urine dipstick examination to rule out a urinary tract infection and provide important indications on glucosuria, a possible first sign of diabetes mellitus but x-ray imaging is not often helpful25 whereas ultrasonography can be useful to evaluate the anatomy.25 In children, neurological imaging of the spine is only needed if there is a suspicion of an abnormality in the pelvis or lumbar spine like a tethered cord or a lipoma.27 Usually, NE in children has a high rate of self-resolution and does not often need an intervention compared to children with daytime wetting with/without night-time wetting who very often have bladder-sphincter dysfunctions, which is in turn correlated with recurrent urinary tract infections.28 Historically, chiropractors have maintained that enuresis responds well to chiropractic adjustments, but scientific literature does not corroborate this.
Enuresis is problematic after the age of five years old.25 According to Thiedke29 the diagnosis of a child up to six years of age should have one or more wetting episodes per month. To explain the neuromusculoskeletal diagnosis, chiropractors theorize that a spinal subluxation of the lumbosacral spine which could affect the bladder and kidneys.8
In chiropractic, a vertebral subluxation is a biomechanical change in the spinal column that causes neurological dysfunction.30 The urinary bladder is supplied by both autonomic and somatic nerves emerging from the lumbopelvic region of the spine.31 Control of the detrusor muscle, which causes bladder emptying, and the external urethral sphincter originates from the S2-S4 segments of the spine.32 Rodnick and Rodnick provide evidence that neurological deficits are restored to their normal function by performing subluxation correction in the areas of the sacral segments of the spine.32 Based on this hypothesis, the relation between the NE in this case and the range of motion of the sacral joints support this reasoning with sacral base joint dysfunction of the patient. The latter had also never recorded any dry nights, without day enuresis and no other possible indicators for renal or neurological pathology and metabolic disease found that could explain her problem. NE has a better prognosis than daytime enuresis.25 No factors such as time, cost and patient preference were reported for this case.
Interventions
The patient received chiropractic care after obtaining the mother’s informed consent. The treatment was based on the diversified technique and consisted of the manipulation of the sacrum using a high-velocity, low-amplitude thrust.33 A posterior-anterior impulse was delivered to the right sacral base in a left side posture position of the patient at each visit. A cavitation of the joint was accomplished by the chiropractor using a left-handed piriformis contact. Soft tissue trigger points were addressed in the psoas muscles, giving direct pressure on the lesser trochanter of the femur on both sides with patient in dorsal decubitus. The patient was scheduled for treatment with a frequency of twice a week for the following four weeks and once a week for six weeks with re-evaluation of the patient’s response to treatment upon each visit. A total of 14 treatments were accomplished and the patient was compliant with the treatment plan. The patient was also asked to perform Kegel exercises during the day at home and/or at school three times a day when she goes to the bathroom. Kegel exercises are used to increase pelvic muscle strength to treat stress, urge, and mixed incontinence.34 According to the chiropractor’s advice, the instructions were to stop the flow of the urine three times and hold it five seconds. A recommendation was also made to change her sleeping position. The child had the habit of sleeping prone; it was suggested that she sleep on one side or on her back to help to maintain the normal lordotic curve of her lumbar spine.
Follow-up and Outcomes
Upon each visit, several outcome measures were collected. These consisted of the volume of urine in the diaper and dry nights and the patient’s overall sense of well-being rated on a global well-being scale. The NE diary yielded some interesting results (Table 2). After the first visit, the child was asked to complete a bedwetting diary and to write in it the possible associated factors/events according to relevance (parties, stressful events and homework) in order to help monitor the number of wet nights.35
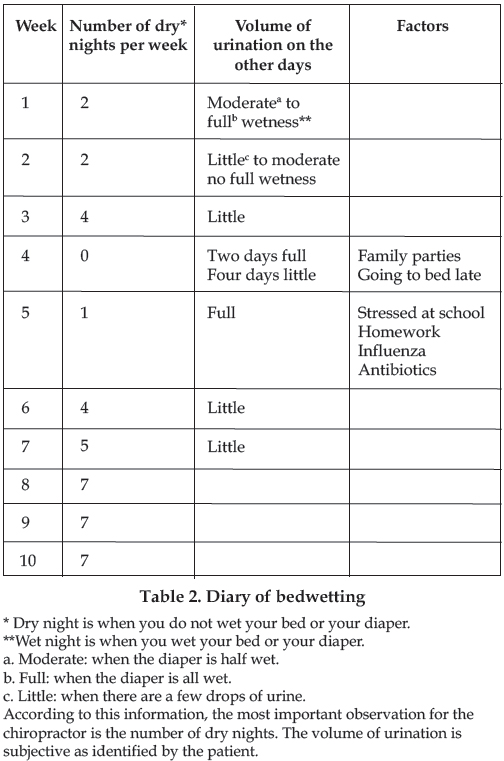
After the first week of treatment, an improvement was noted with the patient reporting two consecutive dry days. A re-evaluation of the right sacral base revealed a greater joint motion and decreased tenderness of the psoas on palpation. Upon the third treatment, the diary reported that she was no longer waking with fully wet pull-up diapers. Upon the fifth treatment, the child had been sleeping without NE for the past four nights. The patient was very happy and proud to show her bedwetting evolution in her diary. Upon the eighth treatment, she reported that the week before, she had regressed and had woken on two consecutive mornings with full diapers followed by a smaller amount of voided night-time urine for four days in a row. Her mother reported that she had actively participated in family parties and that she had gone to bed late on the weekend previous to the regression. On the ninth visit, the mother claimed that the child had resumed night-time voiding frequently that week because she had been stressed by a heavy homework load for school. She had also succumbed to influenza and had been prescribed 10 days of antibiotics. On the 12th to 14th visits, it was reported that the child had been enuresis-free. This had been the longest dry period in the patient’s lifetime. A positive change was noticed in the child whose mood had improved. There was also a resolution of the restriction in the joints of the sacrum upon chiropractic motion palpation. The psoas was completely relaxed, and there was no tension or tenderness noted on palpation.
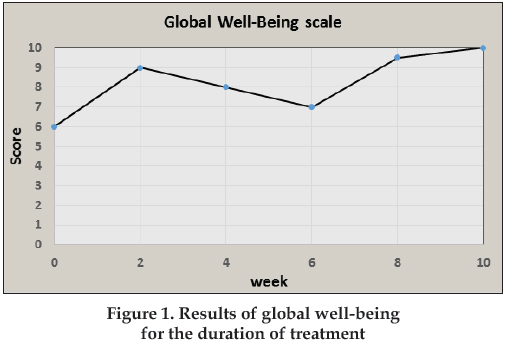
The data collected from the patient’s questionnaire was presented in tabular and graph form in order to track the patient’s progress with each outcome measure over time. The global well-being scale showed a gradual, progressive increase in well-being, with the patient feeling “great” by the end of the treatment (see Figure 1). Throughout the treatment plan, the patient was compliant with self-care recommendations and was doing regular Kegel exercises and was able to sleep on her back. The long-term follow-up at three months displayed continued resolution of NE and the patient’s social life had improved including more frequent sleepovers with friends without the stress and fear of wetting the bed. No adverse events associated with her chiropractic treatments or recommendations were reported by the mother, and the child was always happy to come to the office for her treatment.
Discussion
The objective of this study was to resolve NE in a 10-year-old female after chiropractic care. The interest in presenting this case report was based on previous studies that evaluated the enuresis care among health care professionals. The chiropractors who are most like to encounter patients with NE should have basic knowledge of the condition and the ability to recognize those who got the diagnosis.
Children consult to treat the inconvenience of socially disruptive and emotional stress associated with NE.36,37 When chiropractors receive these patients, they should include conditions like bedwetting in their system survey. When discovered in the written intake or in the interview process, they should take the proper measures to ensure appropriate management. This is the reason why an integrative approach for a child who wets the bed with the inclusion of chiropractic care is encourage.
In this case, a diary was used to evaluate the quantity of bedwetting by using dry, little, moderate and full wetness. Table 2 gives a general indication of the degree of NE experienced by the patient throughout the study period. A decrease in the quantity of wet nights were noted after the first visits and the resolution of bedwetting came about after the 14th visit. We noted that multiples factors affected the pattern of NE with the patient’s response to treatment such as stress factors. Another interesting result was the global sense of well-being. After the entire treatment plan, there was a significant improvement (Figure 1). The patient reported a global feeling of wellness of almost ten on ten, however many life factors can contribute to this. Sleep, social, emotional and chemical disorders can lead to a change in global comfort life too. Future studies may attempt to include these when assessing outcome measures by the use of a variety of additional questionnaires.
Limitations
The strongest limitation of this study is the small sample size because this is the only case. Causality cannot be established in case reports, the reader should not generalize from the presentation of the case. Multiple explanations could explain the beneficial effects reported in the case. Many factors are uncontrolled for this case report, for instance, lifestyle may interfere with the results. These successful outcomes contributing factors may include: placebo effect, natural history, statistical regression and subjective validation. If the assessment of the outcomes following chiropractic care were not documented in the form of diary, then quantifiable improvements would be more difficult. Any events such as homework, holidays and diseases may affect the global sense of well-being around that time of treatment. The author is aware of the low level of evidence that a case report provides, but it is a platform from which to encourage further research and a good tool for the healthcare population to be aware of different approaches for the management of this condition.
Conclusion
Finally, it appears that chiropractic treatment may have a role in the improvement of NE. It is not appropriate to generalize the results to a larger population as this report is a trial based on findings in one person, however suggests the necessity of carrying out a more rigorous and further-designed study which includes control groups in order to sufficiently determine the efficiency of chiropractic treatment for patients with NE.
REFERENCES
1. Humphreys BK, Sulkowski A, McIntyre K, Kasiban M, Patrick AN. An examination of musculoskeletal cognitive competency in chiropractic interns. J Manip Physiol Thera 2007; 30(1): 44-9.
2. Ferrance RJ, Miller J. Chiropractic diagnosis and management of non-musculoskeletal conditions in children and adolescents. Chiropr Ostetopathy. 2010; 18:14.
3. Huang T, Shu X, Huang YS, Cheuk DKL. Complementary and miscellaneous interventions for nocturnal enuresis in children. Cochrane Database Syst Rev 2011; 12CD005230.
4. Forsythe WI, Redmond A. Enuresis and spontaneous cure rate. Study of 1129 enuretics. Arch Dis Child 1974; 49(4):259–63.
5. Glazener CMA, Evans JHC. Desmopressin for nocturnal enuresis in children. Cochrane Database Syst Rev 2002; 3CD002112.
6. Glazener CMA, Evans JHC, Peto R. Tricyclic and related drugs for nocturnal enuresis in children. Cochrane Database Syst Rev 2003; 3CD002117.
7. Deshpande AV, Caldwell PH, Sureshkumar P. Drugs for nocturnal enuresis in children (other than desmopressin and tricyclics). Cochrane Database Syst Rev 2012; 12CD002238.
8. Glazener CMA, Evans JHC, Peto RE. Complex behavioural and educational interventions for nocturnal enuresis in children. Cochrane Database Syst Rev 2004; 1CD004668.
9. Caldwell PH, Nankivell G, Sureshkumar P. Simple behavioural interventions for nocturnal enuresis in children. Cochrane Database Syst Rev 2013; 7CD003637.
10. Glazener CMA, Evans JHC, Peto RE. Alarm interventions for nocturnal enuresis in children. Cochrane Database Syst Rev 2005; 2CD002911.
11. Maternik M, Krzeminska K and Zurowska A, The management of childhood urinary incontinence. Pediatr Nephrol 2015 30:41
12. LeBoeuf C, Brown P, Herman A, Leembruggen K, Walton D, Crisp TC: Chiropractic care of children with nocturnal enuresis – a prospective outcome study. J Manipulative Physiol Ther 1991, 14 (2): 110-115.
13. Reed WR, Beavers S, Reddy SK, Kern G: Chiropractic management of primary nocturnal enuresis. J Manipulative Physiol Ther 1994, 17 (9): 596-600.
14. Eigil Instebø, Reidar P Lystad, Chiropractic Care of an 8-Year-Old Girl With Nonorganic, Primary Nocturnal Enuresis: A Case Report, Journal of Chiropractic Medicine (2016) 15, 47–52.
15. Gemmell HA, Jacobsen BH. Chiropractic management of enuresis: time-series descriptive design. J Manipulative Physiol Ther 1989; 12(5):386–9.
16. Blomerth PR. Functional nocturnal enuresis. J Manipulative Physiol Ther 1994; 17: 335-8.
17. Marko RB. Bed-wetting; two case studies. Chiropr Paediatr 1994; 1: 21-2.
18. McCormick J. Improvement in nocturnal enuresis with chiropractic care: A case study. J Clin Chirop Pediatr 2006; 7(1): 464-465
19. Alcantara J, Weisberg JE. Resolution of nocturnal enuresis and vertebral subluxation in a pediatric patient undergoing chiropractic care: a case report and a review
20. Kreitz BG, Aker PD. Nocturnal enuresis: treatment implications for the chiropractor. J Manipulative Physiol Ther 1994; 17(7):465-73
21. Van Poecke AJ, Cunliffe C. Chiropractic treatment for primary nocturnal enuresis: a case series of 33 consecutive patients. J Manipulative Physiol Ther 2009 Oct; 32(8):675-678
22. Bronfort G, Haas M, Evans R, Leininger B, Triano J. Effectiveness of manual therapies: the UK evidence report. Chiropr Osteopat 2010; 18:3.
23. Gleberzon BJ, Arts J, Mei A, McManus EL. The use of spinal manipulative therapy for pediatric health conditions: a systematic review of the literature. J Can Chiropr Assoc 2012;56(2):128–41
24. Clar C, Tsertsvadze A, Court R, Hundt GL, Clarke A, and Sutcliffe P. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropr Man Therap 2014; 22:12.
25. Bernhard Haid, Serdar Tekgul, Primary and Secondary Enuresis: Pathophysiology, Diagnosis, and Treatment. European urology focus 3 (2017) 198-206.
26. Austin PF, Bauer SB, Bower W, et al. The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the standardization committee of the International Children’s Continence Society. J Urol 2014; 191:1863–5.
27. Pippi Salle JL, Capolicchio G, Houle AM, Vernet O, Jednak R, O’Gorman AM, Montes JL, Farmer JP: Magnetic resonance imaging in children with voiding dysfunction: is it indicated? J Urol 1998, 160:1080-3.
28. E Bakker et al, Voiding Habits and Wetting in a Population of 4332 Belgian Schoolchildren Aged Between 10 and 14 Years, Scand J Urol Nephrol 36: 354–362, 2002
29. American Psychiatric Association: Diagnostic and statistical manual of mental disorders (4th ed, text revision) Washington, DC, American Psychiatric Pub 2000.
30. Kent C. Models of vertebral subluxation: a review. J Vert Sublux Res 1996 August; 1 (1): 1-7.
31. De Groat WC, Yoshimura N. Afferent nerve regulation of bladder function in health and disease. Handb Exp Pharmacol 2009; 194: 91–138.
32. Rodnick A, Rodnick P. Resolution of childhood nocturnal enuresis following subluxation-based chiropractic care: a retrospective case study. J Pediatr Matern and Fam Health 2010 Oct 19; 10(4):159-162.
33. Bergmann TF, Peterson DH, Lawrence DJ. Chiropractic technique: principles and procedures. New York: Churchill Livingstone; 1993.
34. Yamanishi T, Yasuda K, Murayama N, Sakakibara R, Uchiyama T, Ito H (2000) Biofeedback training for detrusor overactivity in children. J Urol 164:1686–1690.
35. Neveus T, Läckgren G, Tuvemo T, Hetta J, Hjalmas K, Steneberg A. Enuresis—background and treatment. Scand J Urol Nephrol Suppl 2000; 206: 1-44.
36. Feehan M, McGee R, Stanton W, Silva PA. A 6 year follow-up of childhood enuresis: prevalence in adolescence and consequences for mental health. J Paediatr Child Health 1990; 26: 75–9.
37. Haggloff B, Andren O, Bergstrom E, Marklund L, Wendelius. Self-esteem before and after treatment in children with nocturnal enuresis and urinary incontinence. Eur Urol 1998; 33: 16-9.
|

