| |
Improvements in a three-year-old girl diagnosed with autism spectrum disorder following a trial of chiropractic care: a case report
By Stephanie K. Makela, DC1
1. Associate chiropractor in private practice, Cedar Rapids, Iowa, USA.
Email: stephaniemakela@hotmail.com
ABSTRACT
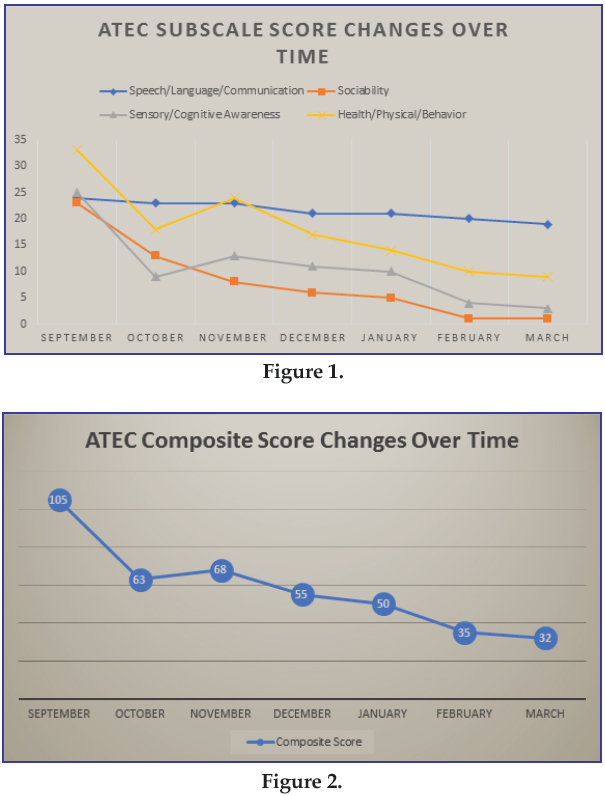
Introduction: This case report describes the effects of chiropractic care on a three-year-old girl who was previously diagnosed with autism spectrum disorder (ASD) experiencing significant language delays as well as delays in other aspects of development including sociability, cognitive awareness, and behavior. The patient was followed for a period of seven months. Presenting Concerns: A three-year-old girl diagnosed with ASD was brought into the chiropractic office by her mother for a trial of chiropractic care. The patient was non-verbal, walked on her toes and was often “off-balance” when walking. Temper tantrums often ensued when the patient was touched by someone. The patient’s mother was hoping for a general reduction of ASD symptoms. Interventions: Chiropractic care commenced and initial treatment plan was to see the patient for 12 visits over a six-week period. The examination had to be tailored to the patient based on her ability and willingness to comply with instructions. Spinal manipulations, also called chiropractic adjustments, were performed using a spring-loaded instrument. Outcomes: The patient’s mother reported improvements in all areas of development over the course of the treatment. Improvements were documented in cognitive awareness, sociability, and behavior, as measured objectively by the Autism Treatment Evaluation Checklist (ATEC), which the patient’s mother completed before treatment and after the initial six weeks. Before starting treatment, the ATEC composite score was 105; after six weeks of care the composite score dropped to 63. The patient’s mother, who was satisfied with the outcomes, chose to continue treatment and completed the ATEC monthly. After seven months of care, the ATEC composite score was a 32. Conclusion: This case report helps to strengthen the relationship between correcting subluxations and the improvements in the myriad of symptoms of children diagnosed with ASD.
Key Words: spinal manipulation, chiropractic adjustment, autism, neurodevelopmental disorders, ATEC
Introduction
Autism spectrum disorder (ASD) is a complex developmental disorder that can cause problems with cognition (thinking), emotion (feeling), language (talking) and sociability (the ability to relate to others). It is a neurological disorder affecting the higher order functions of the brain. The effects of autism and the severity of symptoms are different in each person.1 In 2018, the Centers for Disease Control (CDC) reported that 1 in 59 children are reported as having ASD.2 According to the Center for Disease Control’s Community Report on Autism released in 2016, the economic burden of treatment for individuals nationwide diagnosed with ASD from birth to age 17 was estimated to be between $11.5-$60.9 billion per year in the United States.3
There is no known cure for ASD, and all medical treatments that are offered today are applied on an individual basis to help reduce the symptoms of ASD and support the child’s learning and development. These can include but are not limited to behavior and communication therapies, occupational therapy, family and educational therapies, and medications which can be prescribed to assist with the symptoms that are associated with ASD. Medications are often prescribed to help hyperactivity; behavioral problems are often treated with antipsychotic drugs; and antidepressants may be prescribed for anxiety or anxiety-like symptoms.4
In an article written by Gleberzon on the chiropractic management of children with autism, he broke down the treatment of children with autism into two categories. The first type is Applied Behavioral Analysis (ABA), which primarily concentrates on helping the child master life skills, such as dressing or bathroom habits, by taking complex tasks and breaking them down into smaller parts eventually combining them all in order to complete the entire task.5 The second category covers additional therapies that the child may need such as speech, occupational, or physical therapies, and helping to improve social relationships.5,6
There is limited research done on chiropractic and the management of children with ASD. In 2011, Alcantara, J et al published a systematic review on the topic of chiropractic care and ASD. Included were five articles, including three case reports, one cohort study, and one randomized comparison trial.7 This was followed by Kronau et al in 2016, whose systematic review revealed one uncontrolled, randomized, clinical trial, one case series, and 11 case reports.8 This demonstrates the need for more research regarding the effectiveness of chiropractic care in the treatment and management of ASD, as the majority of the published literature on this topic consists of case reports.
The following case report discusses a three-year-old female patient diagnosed with ASD, who presented in the author’s chiropractic office for a trial of subluxation-based chiropractic care. The patient’s name was changed in this report in order to protect patient confidentiality.
Presenting Concerns
Maggie presented to the author’s chiropractic practice with her mother. Maggie’s mother explained that Maggie was previously diagnosed with Autism Spectrum Disorder. She could not communicate verbally and did not use non-verbal cues (i.e. pointing for basic needs or sign language). The only way that Maggie was able to communicate was through crying and occasionally a guttural sound. The patient’s mother also reported that Maggie did not like to be touched. She stated that occasionally Maggie acted as though she did not notice that she was being touched, but other times, a temper tantum ensued when someone touched her. It was also reported that Maggie would be “off balance” often when on her feet and would run into things when walking or running. Maggie’s mother stated that Maggie walked on her toes 50% of the time.
Clinical Findings
Relevant History
This was the mother’s first pregnancy. She reported that she was taking the anti-nausea drug, Zofran until she was into the third trimester, but discontinued it before she gave birth. Her labor was long, lasting over 24 hours. Her water broke spontaneously after she was admitted into the hospital. Meconium was present in the amniotic fluid. An epidural was administered for pain relief. Due to the inability to coordinate her pushes, both vacuum and forceps were applied during the vaginal delivery. Maggie’s mother reported a large amount of swelling on Maggie’s head after her birth due to the use of the vacuum. The baby presented with a nuchal chord and was cyanotic. Oxygen was immediately administered. The neonate was transported to NICU and retained for two days to monitor her urination, her bilirubin levels and pO2. The hematoma on her head prompted frequent subsequent measurements of head circumference for her first year of life. By the time Maggie reached her first birthday, her doctor was comfortable with her measurements and progressive growth and discontinued the practice. All vaccinations were given on the schedule currently recommended by the American Academy of Pediatrics (AAP).
Maggie’s mother reported that Maggie had a very healthy childhood and had only been on two courses of antibiotics during her lifetime. Maggie had no known allergies and was breastfed until nine months of age. It was reported that Maggie had no issues sleeping and slept around 10 hours per night with minimal disturbances. Maggie had a good appetite and was only a picky eater “occasionally.” Maggie’s mother stated that the child had some repetitive or “stimming” behaviors, the most prevalent one being the flapping of her hands and arms. Maggie also still wore a diaper and was not “potty trained.”
Relevant Co-morbidities and/or Interventions
Maggie was officially given her diagnosis of ASD at 18 months of age, with the official diagnosis coming before her fourth birthday. Maggie then began in-home speech therapy 1-2 times per week until she turned three years old. Concurrently, once Maggie turned two years old, she also attended private speech therapy once per week. Private speech therapy was still ongoing at the time of her first chiropractic appointment. In addition, Maggie started occupational therapy when she was two-and-one-half-years-old where she worked on activities of daily living (ADL’s) such as dressing herself and brushing her teeth. She also started physical therapy at this time because Maggie was walking on her toes 100% of the time as well as running into walls when she walked (See Timeline/Table 1). At the time that the author saw Maggie for the first time at three years old, she was still predominantly toe-walking, but no longer consistently walking into walls. She was unable to independently dress herself or brush her teeth on her own. Her mother was hoping for a reduction of overall symptoms relating to ASD.
Physical Examination Findings
The physical exam was modified based on Maggie’s cooperation. Upon observation, a right head tilt with anterior head carriage and a left rotated pelvis was noted. The patient had an elevated right shoulder when comparing the acromion processes bilaterally. Maggie presented with genu valgus, toeing out/foot flare of the left foot and toe walking. When testing eye movement, patient would not focus on the object that the author was using in order to test the patient’s visual tracking ability. The patient would not allow the author to test any reflexes. The patient had a leg length difference that was noted both when lying supine as well as prone. The left leg was short by 1/2”. This leg length was a functional one, meaning that the leg length difference, based on the position of the individual innominates and the change in the height of the acetabulum, was corrected once the adjustment was completed. An anatomical leg length difference means that there is an anatomical reason for the legs to be different lengths (previous fracture, growth plate issues, etc) and therefore cannot be influenced by a chiropractic adjustment. In Maggie’s case, her leg length difference was functional. Maggie did not make eye contact with the author nor her mother at any time during the examination. In addition, she did not respond to her name being said or called at any point. Muscle hypertonicity was evaluated by the use of static palpation, with the highest tone being in the sub-occipital muscle group. Spinal segment misalignments were determined by the use of motion palpation. An anterior-superior occiput was noted, as well as a right laterality of atlas and a posterior inferior ilium on the left.
Diagnostic Focus and Assessment
Before Maggie’s adjustment, the author had Maggie’s mother fill out the Autism Treatment Evaluation Checklist (ATEC) form so that she could more adequately track Maggie’s progress. The Autism Research Institute in San Diego, California developed the Autism Treatment Evaluation Checklist for the purpose of allowing caregivers to track changes in ASD symptoms over a period of time, which allows practitioners the ability to more easily track the effectiveness of any given treatment.9 The questionnaire is available online and it is free to access as well as score once it is completed. The ATEC measures four areas of the child’s development, including Speech/Language/Communication, Sociability, Sensory/Cognitive Awareness, and Health/Physical/Behavior subscales by asking the parent 77 questions within these subscales. Each area is then given a score, which are then combined to calculate a total score which ranges from 0-180. The higher the total score, the more impairment the child is experiencing. A total score above 104 indicates that the child is severely autistic, scores between 50-104 indicate moderate symptoms, scores between 30-50 indicate that the child may lead a partially independent life, and scores of less than 30 indicate that the child could lead a normal and independent life.9
Therapeutic Focus and Assessment
Chiropractic care commenced with an anticipated treatment plan of 12 visits over a period of six weeks. One of Maggie’s 12 visits was not completed due to a scheduling conflict and it was unable to be rescheduled. In that si week period, Maggie was given a spinal manipulation, also called a chiropractic adjustment, on 11 occasions using a spring-loaded instrument-assisted technique. As outlined above, Maggie’s occiput, atlas, and left ilium were adjusted, if indicated, during each visit. In addition, other vertebral segments were found and corrected as needed.
Follow-up and Outcomes
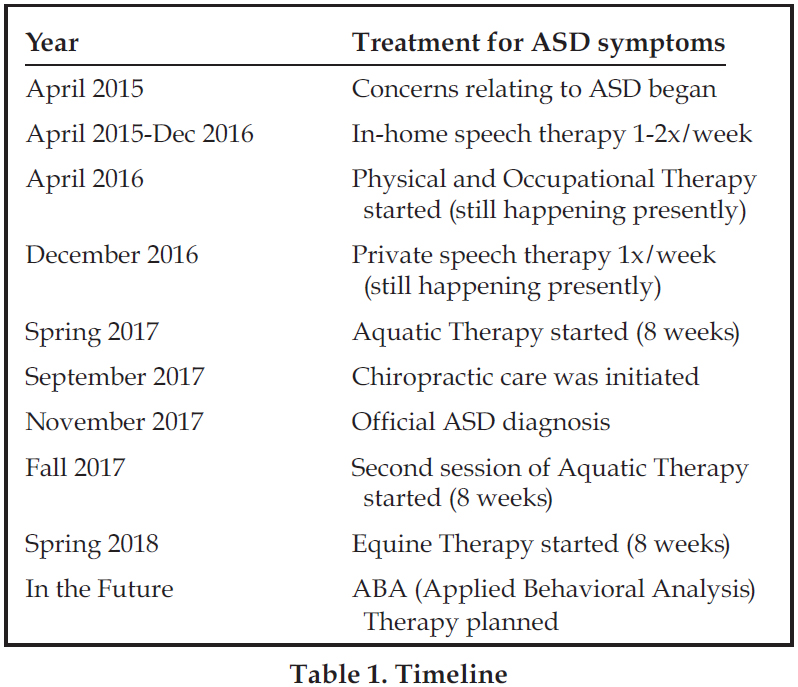
The results of Maggie’s first ATEC resulted in a total composite score of 105. Her speech/language communication score was 23 out of a possible 28. She scored a 23 in the sociability subscale out of a possible 40. In the sensory/cognitive awareness portion, she scored a 25 out of a possible 36 and in the health/physical/behavior section, she scored a 33 out of 75. After the fourth adjustment, Maggie held eye contact with her mom for five seconds. Her mother reported that this was the first time that Maggie made purposeful eye contact with her. At the sixth adjustment, her mother reported that Maggie verbalized what she thought was “dada” for the first time. At visit seven, Maggie’s mother stated that there had been a “big change” in the amount of eye contact that Maggie does now as well as her demeanor being much calmer when they are at home. By visit 10, Maggie started to smile and her mother reported that at home, she has responded much more when hearing voices. At visit 11, Maggie touched the author’s face when the author adjusted her and she held the author’s hand after the adjustment was completed. No adverse reactions to treatment were reported during this time. After six weeks of care, Maggie’s mother completed another ATEC at which time her composite score dropped to a 63. The scores of the subscales consisted of a 23 in speech/language/communication, 13 in sociability, 9 in sensory/cognitive awareness, and 18 in health/physical/behavior.
After completing the follow-up ATEC and going over it with Maggie’s mother, she stated that she was excited about the changes going on with Maggie and wanted to continue with care. At this point, we agreed upon a treatment plan that included Maggie being adjusted two times per week and we would track her progress with the ATEC monthly. Within this next month, there was one week that the author’s did not see Maggie due to Maggie having a virus. The author hypothesized that this break in care could have been part of the reason that her score on the next ATEC increased by 5 points. For all of the following months, the patient was seen on schedule and was compliant following the prescribed treatment plan.
No adverse reactions were seen or reported, and positive progress was documented per the results of the monthly tracking of the ATEC scores (Figures 1 & 2). Significant changes were observed as follows: In mid-December, Maggie’s mother reported that she was laughing more at home. Sometimes the laughter was spontaneous, but other times, she was laughing appropriately at things that were funny. In early January, Maggie signed the word “want” appropriately without being prompted. In early February, it was reported that Maggie was starting to wave “bye-bye” to people more often. By late February, Maggie could recognize all the letters in her name and recognize numbers 1-5. In mid-March, Maggie started to point to things that she wanted and started to express more emotions, including giving hugs and blowing kisses. The patient’s mother was extremely pleased with the progress and the changes that occurred in the patient from the time that she started her care until the present. At any point during the course of her treatment, Maggie’s mother reported that she had no negative reactions to treatment. Maggie is still currently under care.
Discussion
A three-year old girl diagnosed with autism spectrum disorder saw significant improvements in almost all areas of development after six weeks of care. That improvement continued over time as her treatment continued. The only area that did not demonstrate significant improvement was her speech/language/communication. Improvement, although minimal, was seen in how she is now pointing at things which she was not doing at the start of Maggie’s treatment. The improvement was noted subjectively, as reported by Maggie’s mother, as well as tracked objectively from the scoring of the ATEC. Data for this report was tracked for a total of seven months, but improvement continues to be noted, as Maggie is still currently under care.
This case is similar to other case reports published on this topic in that it demonstrates improvements in ASD symptoms after a trial course of chiropractic care. This case is different than other reports that have been published in the literature because most cases only discuss results over a short period of time, whereas the author has tracked improvement over the course of seven months.
Patient perspective
The patient’s mother was thrilled with the progress that Maggie had made with chiropractic care. She stated that her speech therapist, occupational therapist, and physical therapist all had noticed positive changes in Maggie when they worked with her since she had started chiropractic care. They also reported that she was calmer and had a longer attention span.
Conclusion
Current literature suggests that a relationship might be established between adjusting the spine and lessening of symptoms associated with ASD. This case is no exception. However, although promising results are seen, this does not prove a cause-effect correlation. This case study helps to strengthen the relationship between correcting subluxations and the improvements of symptoms of children diagnosed with ASD, however, further studies documenting this relationship are needed. Future studies could investigate whether the patient maintains their ATEC scores without treatment or if they regress after cessation of care.
References
1. American Psychiatric Association [Online]. 2016; Available at https://www.psychiatry.org/patients-families/autism/what-is-autism-spectrum-disorder.
2. CDC. Prevalence of Autism Spectrum Disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR 2018;67(6); 1-23. Available at https://www.cdc.gov/mmwr/volumes/67/ss/ss6706a1.htm.
3. CDC, National Center on Birth Defects and Developmental Disabilities. Community Report on Autism. 2016.
4. Mayo Clinic [Online]. Available at https://www.mayoclinic.org/diseases-conditions/autism-spectrum-disorder/diagnosis-treatment/drc-20352934.
5. Gleberzon, BJ. Chiropractic and the management of children with autism. Clinical Chiropractic 2006 Dec. 9(4):176-181.
6. Noriega A, Chung J, Brown J. Improvement in a 6-year-old child with autistic spectrum disorder and nocturnal enuresis under upper cervical chiropractic care. J Upper Cervical Chiropractic Research Jan 30, 2012.
7. Alcantara J, Alcantara, JD, Alcantara J. A systematic review of the literature on the chiropractic care of patients with autism spectrum disorder. Explore 2011 Nov/Dec 7(6): 384-390.
8. Kronau S, Thiel B, Jakel A, Torsten L. Clinical effects of spinal manipulation in the management of children and young adults diagnosed with autism spectrum disorder—a systematic review of the literature. J Clin Chiropractic Ped 2016; Dec 15(3): 1280-1291.
9. Mahapatra, S.; Vyshedsky, D.; Martinez, S., et al. Autism Treatment Evaluation Checklist (ATEC) Norms: A “Growth Chart” for ATEC Score Changes as a Function of Age. Children 2018; 5(2). doi: 10.3390/children5020025.
|

