| |
Pediatric osteosarcoma of the knee: a case-report
By Jessica Dallaire, DC1
1. Private practice, Chiropratique Mont-Tremblant, Quebec, Canada.
Email : chirotremblant@gmail.com
ABSTRACT
Introduction: The aim of this study is to help chiropractors and other healthcare professionals recognize the signs and symptoms that can lead to the identification of a malignant condition like an osteosarcoma, especially in cases where atypical pain presents in pediatric patients. Clinical features: A 13-year-old boy presented with severe knee pain resulting in the inability to bear weight. There were no obvious causes for the pain that had first developed 24 hours prior to the patient’s visit to the chiropractor. Treatment primarily consisted of administering an x-ray that lead to the discovery of a malignant tumor on the right proximal tibia. Interventions and outcomes: The patient was sent to a pediatric hospital for further investigation which resulted in a diagnosis of primary metastatic osteosarcoma. Treatment consisted of total resection of the tumor, prosthetic reconstruction, and chemotherapy to eradicate the cancer. The patient is not yet in remission; however, there is no visible trace of malignancy. Conclusion: Pediatric malignant tumors are typically very aggressive; therefore, early detection of clinical presentations and timely intervention are crucial to improve the outcomes in pediatric patients with primary metastatic osteosarcoma. This particular patient was seen at the right time and a later diagnosis would have likely impacted his prognosis. This case report provides a good example of when to refer a patient. Articular manipulation in this case would have harmed the patient.1
Key words: case report, osteosarcoma, pediatric cancer, osteogenic sarcoma, pediatric tumor
Introduction
Despite its rarity, osteosarcoma (OS) represents the second most common primary malignancy of bone, with approximately 800 new cases reported in the United States each year. Of these 800 cases, half of them involve the pediatric population,2 and is therefore considered the most common primary malignancy tumor of bone affecting children.3 Chances are that a chiropractor or a healthcare professional will never encounter a case of OS. Nonetheless, it is important that these professionals can properly recognize the signs and symptoms since, in the rare instances where a diagnosis of OS is made, early detection will provide the patient with the best chance of survival. For this reason, this case report will be of particular interest to those professionals who specialize in pediatric care.
An osteogenic sarcoma is characterized by the production of malignant osteoid arising from primitive mesenchymal bone-forming cells.2 42% of OS are reported in the femur (75% distal), 19% in the tibia (80% proximal) and 10% in the humerus (90% proximal). On rare occasions, especially in older adults, OS can develop in the proximal bones like the pelvis (8%) or the skull and jaw (8%). Rapid bone growth appears to be a predisposing factor, which could explain why it is most commonly found in the metaphyseal area, adjacent to the growth plate of long bones and why it happens during the adolescent growth spurt (15-17 years for males and 13 years for females).4 A study, consisting of 962 patients that developed OS between 1981 and 2000, suggested that taller stature is possibly a risk factor for individuals who are 18 years and younger. This is most likely because of their rapid growth velocity, increasing cellular division and resulting in a higher probability of dysfunctional cells.5 Additionally, approximately 1% of people with Paget’s disease will develop an osteosarcoma as a result of the abnormal bone remodeling.6 Other rare genetic disease like the germ-line form of retinoblastoma, Li-Fraumeni syndrome (Germ-line TP53 mutation),7 Rothmund Thomson syndrome, Werner syndrome, Diamond Blackfan anemia and Bloom syndrome will predispose patients to OS. Finally, ionizing radiation exposure is an environmental risk factor that can cause secondary osteosarcoma.8 In United States, the incidence of OS in individuals 20 years and younger is slightly higher in males (5.1 million per year) than in females (4.5 per million per year) as well as a little higher in African American than in Caucasians.4
After confirming a diagnosis of OS by X-ray, magnetic resonance imaging (MRI), blood tests, radionuclide bone scan, biopsy and computed tomography (CT) or DNA testing if necessary,9 a treatment plan is established depending on the grade and stage of the tumor.10 For a high-grade osteosarcoma such as the one being presented in this case study, chemotherapy is generally administered before and after the reconstructive surgery that is carried out to salvage the limb.11 In total, the patient goes through six to 10 months of treatment.12 The survival outlined in the United States SEER database between 1973 and 2004 demonstrated that the relative five year survival rate for young-onset osteosarcoma was 61.6%. Overall, osteosarcoma survival rates improved with each decade up until the 1990s, and then little thereafter.13
Clinical features
A 13-year-old Caucasian boy presented to a chiropractor with right knee pain after playing soccer the previous evening. No obvious trauma was sustained during the soccer game that could easily explain the onset of pain. The source of the pain was located on the proximal tibiofibular articulation and on the patella, and radiated caudally to the ankle. The patient characterized it as deep and intense pain that felt like electric shocks. In the weeks leading to the onset of pain, the patient felt normal and experienced no nausea, loss of appetite or fatigue. Additionally, the pain was not waking him at night.
Clinical findings
Relevant history, comorbidities and/or Interventions
With the exception of suffering from immune thrombocytopenic purpura at the age of one and being gluten intolerant, the patient led a very healthy lifestyle. In the year leading up to his diagnosis, the patient was seen four times by the same chiropractor for a mild concussion and for fat pad syndrome on the right foot. Both conditions were resolved.
Physical examination findings
Upon physical examination, the patient could not bear weight on the affected leg, and consequently presented with a limp. The extension, internal and external rotation of the knee were normal, however he could not flex more than 30 degrees actively and passively. The patient was also unable to perform resisted flexion or extensions and the active or passive range of motion of the right ankle all caused pain (flexion, extension, inversion and eversion). Finally, when asked to resist extension of the toes and ankle, the patient was unable to complete the task. The neurological exam, including fine touch and pain of L1 to S1, found nothing abnormal. Patellar and achille reflexes were normal. Vibration on the proximal tibiofibular articulation was painful. Upon further observation, minor edema was noted with no bruising. When examining the patient using light palpation, any contact of the proximal fibula and tibia resulted in severe pain. The palpation of the patella, quadriceps (including the patellar tendon), hamstrings and gastrocnemius were not painful.
Diagnostic focus and assessment
The two first working differential diagnosis were a sprain of the right proximal interosseous membrane by overuse of the articulation and a fracture of the lateral tibial plateau. Kinesiotaping was done to help drain the swelling and to stabilize the knee join. No articular manipulation was carried out on the knee, ankle or spine. The patient was sent for X-rays, as the symptoms were too severe, to eliminate a fracture possibility. The chiropractor recommended the patient be fitted for crutches to avoid weight bearing until a firm diagnosis was reached. The X-rays showed a 5x4x4 cm lesion in the proximal metaphyseal area of the right tibia. It was mixed (lytic and blastic) with cortical destruction, accompanied by an interrupted periosteal reaction. Based on the results, the radiologist suspected a tumor (Figs 1-2), and immediately recommend the chiropractor to refer the patient to a children’s hospital for further testing. The patient’s family physician was also notified.

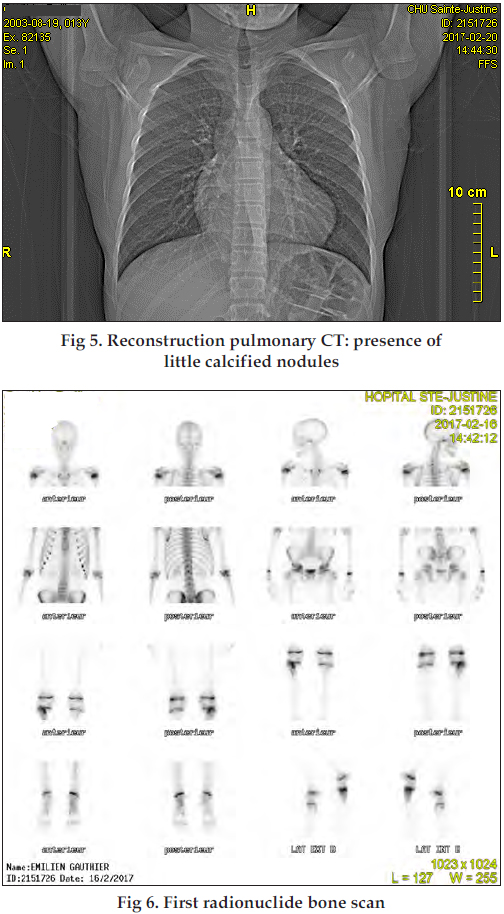
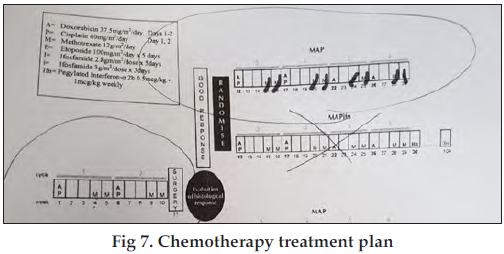
That same week, an MRI (Figs 3-4), a pulmonary X-ray (Fig 5), a biopsy and a radionuclide bone scan (Fig 6) were carried out. The pulmonary x-ray showed little blastic spots on the four lobes and the other tests confirmed the first hypothesis. The diagnosis of primary metastatic osteosarcoma came two weeks following the patient’s initial x-ray. The orthopedic surgeon would not provide a prognosis due to the highly variable responses to chemotherapy and limb surgery among patients.

Therapeutic Focus and Assessment
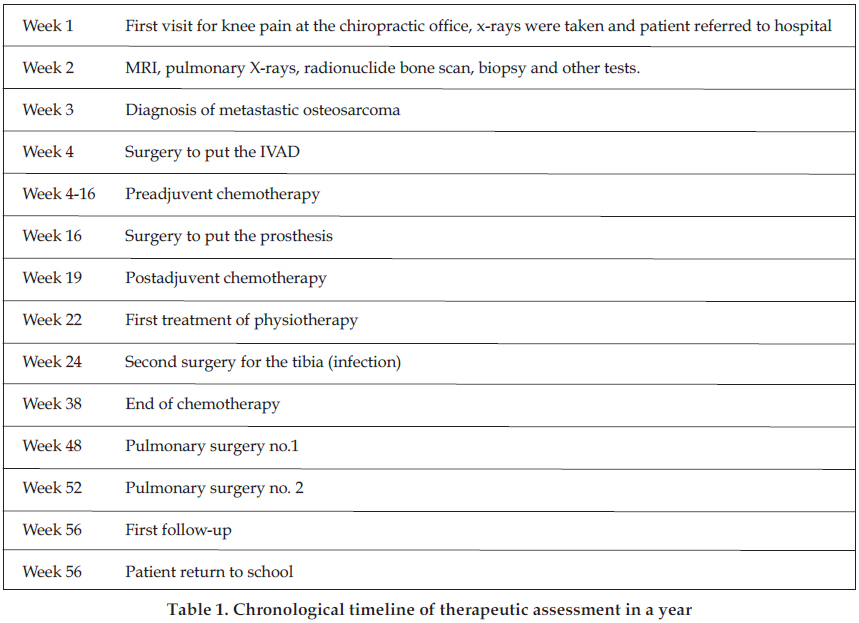
An implantable venous access device (IVAD) was inserted to allow multiple doses of medication to be administered as needed. Subsequently, the patient experienced an infection caused by the catheter and two other surgeries were performed in order to resect the original catheter and reinstall a new one. A month and a half after the diagnosis, the patient started pre-adjuvant chemotherapy. A combination of Doxorubicin, Cisplatin and Methotraxte were used over a period of 29 weeks (Fig 7). While the literature has yet to reflect the hypothesis that neoadjuvant chemotherapy results in better survival rates over postoperative chemotherapy alone,11 chemotherapy combine with surgery increase survival probabilities from 10-20% for a surgery alone to more than 60% for a multimodal treatment.3 The chemotherapy was very difficult, as the young patient developed oral mucositis that led to further complications associated with the patient’s ability to eat and drink. Three months later, the pediatric orthopedist resected the primary tumour and installed a prosthesis, which is the treatment of choice for optimizing the balance between preservation of form and function of the limb and adequate oncological clearance.14 This megaprothesis, designed by Stanmore Implants, was a cemented femoral and tibial stem with a standard SMILES rotating hinge knee for the joint (Figs 8-12).

Fortunately, they were able to resect 13 cm, constituting 97% of the tumour. According to the orthopedist, these are exceptional surgery result, as her goal was 90%. However, they had to reopen two months later because he developed an infection. This time, they used a PICO negative pressure wound therapy to be sure that the wound would heal without oxygen, decreasing the risks of infection. A patient is at the highest risk for infection after proximal tibia resection due to the poor soft tissue coverage. Furthermore, the large exposure of tissues and extensive dissection across vascular distributions also contributes to a high risk of infection.15 The second part of chemotherapy started less than a month after the first limb surgery and finished four months later (fig 7). This time, they waited that the buccal mucositis healed properly before giving another round of medication. Physiotherapy was carried out at the hospital two times a week and consisted of passive extension of the knee. No chiropractic treatment or manipulations were performed, as the patient was usually at the hospital or at home for chemotherapy recovery. In addition, as Clar et al reported, clinical effectiveness of manual therapy for osteosarcoma is negative.1,16
Follow-up and outcomes
Nearly a year after the first consultation, the patient’s surgeons performed a thoracotomy on the left lung for the resection of pulmonary metastasis.17 They found no metastasis, only ossified granulomas. They did a thoracoscopy for the other lung a month later and found the same thing. Overall, the response to the chemotherapy was good and because they succeed in retrieving the vast majority of the primary tumour, the prognosis of the young boy was better than expected. The literature outlines that a patient’s prognosis is dependent upon several factors. Based on a 10 years survival, factors include the patient’s age (40 years and more: 41,6% and less than 40 years 60,2%), the tumor site (axial: 29,2%, limb: 61,7%), primary metastases (yes: 26,7% no: 64,4%), size of the tumor (more than one third: 52,5%, less: 66,7%) and the location on the limb (proximal: 49,3%, other: 52,5%). The response to chemotherapy (poor: 47,2% good: 73,4%) and surgical outcomes (incomplete: 14,6% complete: 64,8%) are other good prognostic factors.18-21 Given this data, one can conclude that there is more than 60% chance there will not be a recurrence of cancer over the next 10 years of his life.
The patient is now regaining function of the knee and healing from everything. There is no visible trace of cancer in is system. He has lost high frequencies in his audition but it is not significant. He will still go to physiotherapy two or three times a week for at least a year. He will have follow-up every months for the first six months, than each three months for the next two years. Then, he will be seen every six months for the following two years. After five years, he will be transferred for an adult follow up and, hopefully, will be in remission by then.
Discussion and limitations
This case report is not a chiropractic case per se and is not meant to augment or improve treatment options for osteosarcoma. Survival rate has been the same since 1990 and more research should be done in this direction to improve the overall prognosis for these patients.13 It is also limited because it is a single case, so it cannot be generalized.22
That said, this case study can help provide valuable information on a condition that, while rare, could present to a chiropractor’s office. It could be especially useful to those professionals who specialize in the care of pediatric patients.
To reiterate, this primary osteogenic sarcoma commonly appears as sporadic intense pain in a long bone, with a predilection for the knee, usually caused by stretching of the periosteum. Pain, when severe and sudden, could also result from weakening of the bone and development of stress fractures. Up to 15% of pediatric patients will present a pathological fracture.23 Pain may worsen at night or with activity and can present local tenderness and a warm palpable mass. Increased skin vascularity may be palpable and pulsations may be detectable too.24 There is a decreased range of motion of the joint and it can lead to a limp if the lower extremities are affected. As we saw in this case, it can affect also the nearest articulations by decreasing their range of motion or their muscle resistance. Risk factors like age (15-19) or a recent grow spurt, when putted together with the previous symptoms should flag the need for extensive testing.3 It is also important for chiropractors that administer X-rays in their office to familiarize themselves with the radiological traits of OS. X-ray results should be examined for one or more of the following indications: medullary destruction and cortical bone interruption, aggressive periosteal reaction (e.g., codman triangle), a sunburst or a lamellated reaction (more seen in Ewing’s sarcoma) and a soft tissue mass. The tumour will appear fluffy or cloudy and reflects a combination of bone production and calcified matrix.25,26 The differential diagnoses to consider are other malignant tumor like Ewing’s sarcoma (differentiated by radionuclide bone scan),27 chondrosarcoma, rhabdomyosarcoma, leiomyosarcoma, osteogenis lymphoma, bone metastasis (generally 40 yo and older) and other conditions like eosinophilic granuloma (histiocytosis), big cells tumour, aneurysmal bone cyst and osteomyelitis.28 The radiological apparence of a low-grade osteosarcoma may also be confused with fibrous lesions like fibromatosis and fibrous dysplasia and, in certain circumstances, can only be differentiated by DNA testing (MDM2 and CDK4).29 OS can also be mistaken with other diagnosis like Paget’s disease, non-ossifying fibroma, myositis ossificans, fracture callus, ossifying hematoma, osteochondroma, desmoplastic fibroma, osteoma and giant bone island.30,31 On a clinical plan, a study of 102 patients diagnosed with OS showed that there was a broad spectrum of misdiagnoses by medical doctor. The most common diagnosis was tendinitis, which was the case for 32 patients.24 According to Robert Grimer, who studied 1,460 patients with newly diagnosed sarcomas, the median duration of symptoms from first patient-identifiable abnormality to diagnosis is 16 weeks.28 Fortunately, in this particular case study, the severity of the knee pain experienced by the patient led to the immediate decision to order X-rays.
Conclusion
Because 18% of OS had already spread at the time of diagnosis32 and that the metastasis had a very poor prognosis, as seen above18, early diagnosis is incredibly important.33 It is hoped that this case study will help contribute to the clinical practice guidelines of when not to manipulate an articulation of a pediatric patient and rather refer for extensive testing.
References
1. Clar et al. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropractic & Manual Therapies 2014; 22:12.
2. Rejniak KA, Lloyd MC, Reed DR, Bui MM. Diagnostic assessment of osteosarcoma chemoresistance based on Virtual Clinical Trials. Med Hypotheses 2015; 85:348–354.
3. The ESMO / European Sarcoma Network Working Group. Bone sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up, Annals of Oncology 2014; 25:113-123.
4. The Epidemiology of Osteosarcoma. Pediatric and Adolescent Osteosarcoma. Texas: Springer; 2009.
5. A. Longhi, A. Pasini, A. Cicognani et al.Height as a risk factor for osteosarcoma. Journal of Pediatric Hematology/Oncology 2005; 27:314–318.
6. Hansen MF, Seton M, Merchant A. Osteosarcoma in Paget’s disease of bone, J Bone Miner Res 2006;21:58-63.
7. Savage et al. Germ-line genetic variation of TP53 in osteosarcoma. Pediatric Blood & Cancer 2007; 49:28-33.
8. Savage SA, Mirabello L. Review artice: Using epidemiology and genomics to understand osteosarcoma etiology. Sarcoma 2011:1-13.
9. Dujardin et al. MDM2 and CDK4 immunohistochemistry is a valuable tool in the differential diagnosis of low-grade osteosarcomas and other primary fibro-osseous lesions of the bone. Modern Pathology 2011; 24:624-637.
10. Meyer JS, Nadel HR, Marina N, et al. Imaging guidelines for children with Ewing sarcoma and osteosarcoma: a report from the Children’s Oncology Group Bone Tumor Committee. Pediatr Blood Cancer 2008; 51:163-170.
11. Goorin AM, Schwartzentruber DJ, Devidas M, et al. Presurgical chemotherapy compared with immediate surgery and adjuvant chemotherapy for non metastatic osteosarcoma. J Clin Oncol 2003; 21:1574-1580.
12. Carrle D, Bielack SS. Current strategies of chemotherapy in osteosarcoma, Int Orthop 2006;30:445-451.
13. Mirabello L, Troisi RJ, and Savage SA. Osteosarcoma incidence and survival rates from 1973 to 2004: data from the surveillance, epidemiology, and end results program. Cancer 2009; 115:1531–1543.
14. Akshay Tiwari. Current concepts in surgical treatment of osteosarcoma. J Clin Orthop Trauma 2012;3:4–9.
15. Graci C, Maccauro G, Muratori F, Spinelli M.S, Rosa M.A, Fabbriciani C. Infection following bone tumor resection and reconstruction with tumoral prostheses: a literature review. Int J Immunopathol Pharmacol 2010; 4:1005–1013.
16. Wu PK, Chen WM, Lee Ok, Chen CF, Chen TH. The prognosis for patients with osteosarcoma who have received prior manipulative therapy. J Bone Joint Surg – British 2010 ;92:1580-1585.
17. Rusch V.W. Pulmonary metastasectomy. Current indications. Chest 1995; 107:322–331.
18. Bielack SS, Kempf-Bielack B, Delling G, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols, J Clin Oncol 2002; 20:pg. 776-790.
19. Kim MS et al. Initial tumor size predicts histologic response and survival in localized osteosarcoma patients. J Surg Oncol 2008; 97:456-461.
20. Wilkins, RM, Cullen, JW, Odom, L et al. Superior survival in treatment of primary non-metastatic pediatric osteosarcoma of the extremity. Ann Surg Oncol 2003; 10:498–507.
21. Grimer RJ. Size Matters for Sarcomas. Ann R Coll Surg Engl 2006; 88:519–524.
22. Nissen T and Wynn R. The clinical case report: a review of its merits and limitations. BMC Res Notes 2014; 7:264.
23. Picci P. Osteosarcoma (Osteogenic sarcoma). Orphanet J Rare Dis 2007; 2:4.
24. Widhe B, Widhe T. Initial symptoms and clinical features in osteosarcoma and Ewing sarcoma. J Bone Joint Surg Am 2000; 82:667-674.
25. Murphey MD, Robbin MR, Mcrae GA et-al. The many faces of osteosarcoma. Radiographics 1997; 17:1205-31.
26. Yarmish G, Klein MJ, Landa J et-al. Imaging characteristics of primary osteosarcoma: nonconventional subtypes. Radiographics 2010;30 :1653-72.
27. Giammarile F, Chauvot P. Place de la scintigraphie osseuse dans les tumeurs osseuses primitives de l’enfant. Médecine Nucléaire, Imagerie fonctionnelle et métabolique 2001;25:227-232.
28. Grimer RJ, Carter SR, Spooner D, et al. Diagnosing musculoskeletal tumours. Sarcoma 2001; 5:89–94.
29. Dujardin et al. MDM2 and CDK4 immunohistochemistry is a valuable tool in the differential diagnosis of low-grade osteosarcomas and other primary fibro-osseous lesions of the bone. Modern Pathology 2011; 24:624-637.
30. Bertoni F, Bacchini P, Fabbri N, et al. Osteosarcoma. Low-grade intraosseous-type osteosarcoma, histologically resembling parosteal osteosarcoma, fibrous dysplasia, and desmoplastic fibroma. Cancer 1993;71: 338–345.
31. Franchi A, Bacchini P, Della Rocca C, et al. Central low-grade osteosarcoma with pagetoid bone formation: a potential diagnostic pitfall. Mod Pathol 2004; :288-291.
32. Marko T, Diessner B and Spector L. Prevalence of metastasis at diagnosis of osteosarcoma: an international comparison. Pediatr Blood Cancer 2016; 63:1006–1011.
33. Rasmussen C et al. Survival and prognostic factors at time of diagnosis in high-grade appendicular osteosarcoma: a 21 year single institution evaluation from east Denmark. Acta Oncol 2018;57: 420-425.
|

