| |
What is the evidence that chiropractic care helps sub-optimal breastfeeding?
By Christina N. Edwards and Joyce Miller, BA, DC, PhD
Introduction
Breastfeeding is regarded as the optimal method of neonatal and infant nutrition.1 The long and short term benefits to the mother-infant dyad are well documented; for the mother, breastfeeding has been attributed to a reduction in breast and ovarian cancer and diabetes.2 The benefits of early initiation of breastfeeding for the neonate is a significant increase in his/her immune response, providing protection against infection and reducing infant mortality.1
Exclusive breastfeeding for the first six months has been associated with lower rates of gastroenteritis, respiratory tract infections, otitis media, eczema and asthma in infants.3 Long term, children who are breastfed are less likely to be obese, perform better on intelligence tests at school, and progress to obtain higher income in adult life.2 A report commissioned by UNICEF UK in 2012 concluded that for just five illnesses, a moderate increase in breastfeeding would save the NHS £40 million, and tens of thousands GP appointments and hospital admissions.3
Despite growing evidence that breastfeeding improves the health and survival of women and children, and contributes to human capital development,2 every country in the world fails to meet recommended breastfeeding standards.1
Therefore, identification and resolution of factors that contribute to sub-optimal feeding is vital in order to improve breastfeeding continuation. The majority of interventions focus attention on the mother. However chiropractors who see pediatric patients have long purported their role in addressing the biomechanical dysfunctions in the infant which may contribute to sub-optimal breastfeeding (SIB).4
Chiropractors are frequently asked about the evidence base for manual intervention for this problem. Therefore, it was important to review the relevant clinical research for this type of care. It was also considered that it was necessary to investigate what types of studies have been done in order to determine whether it would be appropriate or not to design a randomized controlled trial. Other authors have investigated the wider research stemming from all types of manual therapy.4 Their research question was, “Have manual interventions been used to correct infants’ musculoskeletal dysfunctions thought to be linked to suboptimal breastfeeding?” As such, theirs was a scoping review that included all types of manual therapies. The purpose of this current review was to be specific to the investigation of chiropractic clinical care for this condition. It was considered that other types of therapy, particularly osteopathy, may supply care, though often under quite different circumstances.
Specifically, osteopathy is a medical profession and as such, often has much earlier exposure to the patient, often in the hospital. Therefore, they also have access to every type of medical procedure and equipment, so there is no fear of harm, as any procedure is easily remedied in that environment. Almost all of chiropractic care is provided in outpatient settings. The purpose of this review was to find and evaluate the types of clinical studies that have been done in the arena of chiropractic care for suboptimal infant breastfeeding, in order to determine whether a RCT was an appropriate next step. There was no attempt to do a Systematic Review or a Meta-analysis.
Background
The WHO recommends breastfeeding initiation within an hour of birth, exclusively for the first six months and continued alongside appropriate foods up to two years of age and beyond, to achieve optimal health, growth and development.5
Often however, despite optimal hospital support, breastfeeding fails due to the infant’s inability to feed. Biomechanical causation, as a result of structural restrictions or birth trauma, can contribute significantly to suboptimal feeding and in these cases, a referral to a musculoskeletal specialist, such as a chiropractor, for structural treatment may be beneficial.7
A number of studies have attempted to identify the factors contributing to suboptimal feeding and determine the most effective package of interventions to influence breastfeeding duration. The purpose of this study was to investigate the available literature on the accessible services of chiropractic care, alone or as part of multidisciplinary care in their support and resolution of nursing difficulties, and the impact on breastfeeding continuation in the mother-infant dyad. The goal was to determine whether there was sufficient background evidence to ground a higher level randomized trial.
Method
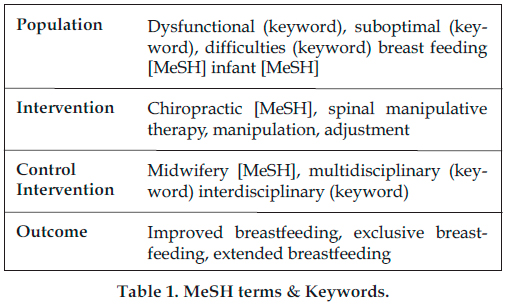
A search of electronic databases relevant to medical and allied health professions, was conducted to review published literature on suboptimal breastfeeding in infants. PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Index to Chiropractic Literature (ICL) and the Cochrane Library were searched. Medical subject heading (MeSH) terms, keywords, natural language terms were combined together in the appropriate Boolean combinations in the search strategy. Spelling variants were also used as it was found that by hyphenating the confound verb “breastfeeding” to “breast-feeding”, or separating it into two individual words (“breast feeding”), very different results were generated. The strategy included terms referring to the population studied, the intervention analysed by the study and the control intervention (Table 1).
Selection Criteria Employed
Primary studies that addressed or described chiropractic or chiropractic/multidisciplinary care of breastfed, infant, human participants were included. All study designs were included with no restriction in terms of publication or date. Only articles published in the English language were included.
Results
104 studies were identified during the electronic search process. A further three papers were received by personal communication with study authors. Of the 107 studies sourced, 26 duplicate records were removed and the remainder screened by title and abstract for relevance. Twelve studies were retrieved as full text articles and their content assessed for additional references meeting the inclusion criteria. A total of ten records that included chiropractic care were appraised to determine their methodological quality using appraisal checklists relevant to the study design (see Table 2 for individual study results and level of critical appraisal).
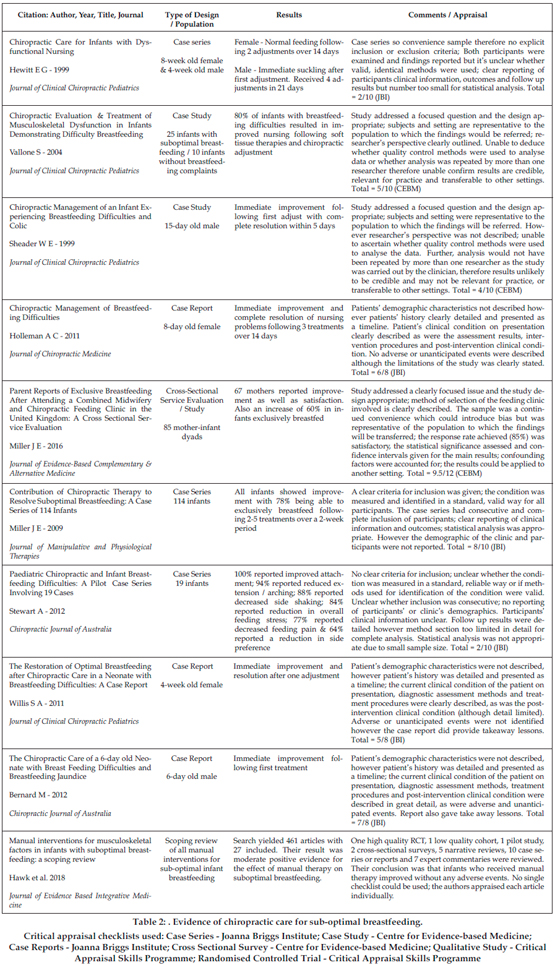
Ten records were reviewed, all demonstrating a low to moderate level of evidence with nine being case series or case reports.4,8-16 In all, a total of 541 newborns, mothers reported improved breastfeeding after chiropractic care.8-16 As well, there was some evidence that collaboration between chiropractors and midwifery teams10 resulted in improved and even sustained breastfeeding.
All of these individual papers were included in Hawk et al’s scoping review4 who found that there is moderate positive evidence for the use of manual therapy for suboptimal breastfeeding.
Discussion
The aim of this review was to investigate the impact of chiropractic care on the continuation of breastfeeding in the mother-infant dyad to determine whether there was sufficient evidence to under-pin a randomized trial. Evidence of benefit for chiropractic care for the breastfeeding dyad exists only at low-to-moderate-level. This is at least partly because it must be considered unethical to include infants with suboptimal breastfeeding into a high level randomized controlled trial where some children would be allocated to a non-treatment group. If there is any evidence of assistance, infants should be allowed to be treated because the benefits of breastfeeding are so key to long-term health.
Still, randomized trials must be done because there is a distinct lack of high-level evidence available on the effects of chiropractic intervention on suboptimal breastfeeding. That which exists comes mostly from cohort studies and case series featuring few participants, relying heavily on clinical experience and anecdotal evidence. Despite the trend towards resolution of breastfeeding difficulties, with all cases reporting an improvement in the infant’s nursing habits, most papers have too much bias to add significantly to the evidence base. Only because of the larger number of cases and the prospective management, one cohort study suggested significant clinical benefit of chiropractic care as a sole disciplinary intervention to resolving breastfeeding difficulties.8 That cohort study reviewed 114 medically-referred cases of infants who had received chiropractic treatment for infant biomechanical dysfunctions relating to suboptimal feeding. Their study reported improvement noting 78% being able to exclusively breastfeed after 2-5 treatments. While the results appear impressive, without a control group, the study is only able to suggest potential links with chiropractic care in the resolution of breastfeeding dysfunction but unable to provide strong evidence. This type of study cannot determine cause and effect due to the lack of a control group and strongly biased results based on reports of maternal perceptions.
A study with equally impressive results (80% recovery rate) by Vallone9 included a group of ten infants without breastfeeding difficulties, indicating early efforts to provide comparison groups.
Likewise, only moderate-level evidence was available to support a combined midwifery and chiropractic intervention. Miller et al in 201610 showed significant improvement in sustained breastfeeding to six months with an interdisciplinary intervention. This is biologically plausible as literature has shown that a traumatic birthing process often results in some form of physical dysfunction in infants, causing imbalance to the spine and muscles of mastication.17 It is thought that even a ‘normal’ birth causes trauma to the infant due to the complicated assortment of compression, contraction, torque and traction during the process.18
Correction of the bio-mechanical disturbance in the infant and provision of one-to-one personal support to assist with maternal concerns, such as positioning, resulted in 93% of mothers reporting an improvement in feeding, with 60% exclusively breastfeeding after intervention.10
However, it could be argued that considerable bias is present in that research and all studies in this review where mothers have sought assistance with breastfeeding difficulties. Intention to breastfeed for a prolonged period has been recognized in literature as a predictor of exclusive and extended breastfeeding.19 These mothers are considered to be a highly motivated population and, therefore, not indicative of the general, wider populace.
While observational studies are useful in assessing treatment outcomes where it may be impractical or unethical to carry out an RCT (for example the provision or withholding of breastfeeding interventions), they cannot provide evidence of actual effectiveness of the treatment, but only anecdotal evidence.
That said, this is a common professional and maternal choice for patients with this condition and because the therapy is safe,20 a trial of treatment is appropriate. Because there is evidence of safety of chiropractic care for the infant, and there is some baseline evidence for benefit to the breastfeeding dyad, there is sufficient support to study the problem with a randomized comparison trial.
Limitations
Only studies in the English language were considered for selection, which may have limited the number of studies assessed.
This review may have failed to consider all confounding variables. Literature identifies there are many predictors of breastfeeding.21 Equally, there is a wide range of non-modifiable factors that can lead to early cessation of breastfeeding, which cannot be controlled or altered clinically. These variables will undoubtedly impact on results, irrespective of the quality of evidence.
Conclusion
Both chiropractic care alone and in a multi-disciplinary setting appear to help sub-optimal breastfeeding but are supported by the lowest levels of scientific evidence and, as such, no statistical significance can be drawn from the positive results reported. Higher quality studies are required to fully determine the cause and effect of such interventions on sub-optimal breastfeeding. However, it must be stated, that since these interventions are safe for the infant and mother, a therapeutic trial is appropriate for these difficult cases. These studies can form a basis upon which to develop a randomized comparison trial.
References:
1. World Health Organization, 2018. Exclusive breastfeeding. Geneva: World Health Organization. Available from: http://www.who.int/nutrition/topics/exclusive_breastfeeding/en/ [accessed 05.01.18]
2. Victora, C. G., Bahl, R., Barros, A. J. D., França, G. V. A., Horton, S., Krasevec, J., Murch, S., Sankar, M. J., Walker, N. and Rollins, N. C., 2016. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet, 387 (10017), 475-490.
3. Renfrew MJ, Pokhrel S, Quigley M, McCormick F, Fox-Rushby J, Dodds R, Duffy S, Trueman P, Williams T (2012) Preventing disease and saving resources: the potential contribution of increasing breastfeeding rates in the UK [online]. London: UNICEF UK Baby Friendly Initiative
4. Hawk C, Minkalis A, Webb C, Hogan O, Vallone S. Manual interventions for musculoskeletal factors in infants with suboptimal breastfeeding: a scoping review. J Evid Based Integr Med 2018;23:1-12. https://journals.sagepub.com/doi/10.1177/2515690X18816971
5. Perelka, E. R., 1986. BREAST FEEDING - BUILDING A BETTER BABY MOTHER NATURE’S WAY. Journal of Chiropratic, 23 (12), 24-27.
6. World Health Organization, 2003. Global Strategy for Infant and Young Child Feeding [online]. Geneva: World Health Organization. Available from: http://www.who.int/mediacentre/factsheets/fs342/en/ [accessed 31.10.17]
7. Vallone, S., 2016. Evaluation and treatment of breastfeeding difficulties associated with cervicocranial dysfunction: A chiropractic perspective. Journal of Clinical Chiropractic Pediatriacs, 15 (3), Online access only p 1301-1305.
8. Miller, J. E., Miller, L., Sulesund, A. K. and Yevtushenko, A., 2009. Contribution of chiropractic therapy to resolving suboptimal breastfeeding: a case series of 114 infants. Journal of Manipulative Physiological Therapeutics, 32 (8), 670-674
9. Vallone S. Chiropractic evaluation and treatment of musculoskeletal dysfunction in infants demonstrating difficulty breastfeed-feeding. J Clin Chiropr Pediatr. 2004;5:349-366.
10. Miller, J., Beharie, M. C., Taylor, A. M., Simmenes, E. B. and Way, S., 2016. Parent Reports of Exclusive Breastfeeding After Attending a Combined Midwifery and Chiropractic Feeding Clinic in the United Kingdom: A Cross-Sectional Service Evaluation. Journal of Evidenced-Based Complementary Alternative Medicine, 21 (2), 85-91.
11. Bernard, M., & Alcantara, J. (2012). The Chiropractic Care of a 6-day-old Neonate with Breastfeeding Difficulties and Breastfeeding Jaundice. Chiropractic Journal of Australia, 42(3), 108-113.
12. Hewitt, E. G. (1999). Chiropractic care for infants with dysfunctional nursing: A case series [case report]. Journal of Clinical Chiropractic Pediatrics, 4(1), 241-244.
13. Holleman, A. C., Nee, J., & Knaap, S. F. (2011). Chiropractic management of breast-feeding difficulties: a case report. Journal of Chiropractic Medicine, 10(3), 199-203.
14. Sheader, W. (1999). Chiropractic Management of an Infant experiencing Breastfeeding Difficulties and Colic: A case Study. Journal Of Clinical Chiropractic Pediatrics, 4(1), 245-247.
15. Willis, S. A. (2011). The restoration of optimal breastfeeding after chiropractic care in a neonate with breastfeeding difficulties: A case report. Journal of Clinical Chiropractic Pediatrics, 12(1), 873-875.
16. Stewart A. Pediatric Chiropractic and Infant Breastfeeding Difficulties: A Pilot Case Series Study involving 19 Cases. Chiropr J Aust. 2012;42:98-107. 26. Bernard M, Alcantara J. The Chiropractic Care of a 6 Day old.
17. Smith, L. J., 2007. Feature: Impact of Birthing Practices on the Breastfeeding Dyad. Journal of Midwifery and Women’s Health, 52, 621-630.
18. Rabelo, N. N., Matushita, H. and Cardeal, D. D., 2017. Traumatic brain lesions in newborns. Arquivos De Neuro-Psiquiatria, 75 (3), 180-188.
19. Donath, S. M. and Amir, L. H., 2003. Relationship between prenatal infant feeding intention and initiation and duration of breastfeeding: a cohort study. Acta Paediatrica, 92 (3), 352-356.
20. Todd AJ, Carroll MT, Robinson A and Mitchell EKL, Adverse events due to chiropractic and other manual therapies for infants and children: A review of the literature. Journal of Manipulative and Physiological Therapeutics,2015;38(9):699-712l https://doi.org/10.1016/j.jmpt.2014.09.008 (Accessed 04/21/19).
21. Hector, D., King, L., Webb, K. and Heywood, P., 2005. Factors affecting breastfeeding practices: applying a conceptual framework. New South Wales Public Health Bulletin, 16 (3-4), 52-55.
|

